"You need to change this"
The prior way I chose to treat as a pelvic health therapist was unethical.
At the time, I was treating men within two weeks of their prostatectomy, yet I would not typically offer this same education early to women after hysterectomy or after cesarean section – until they complained of issues.
I would allow their surgeons to dictate when they could start physical therapy despite what I knew about early recovery and healing.
I will never forget one woman in particular who was referred to me for physical therapy 8 weeks after her hysterectomy.
She had to ask her doctor for the referral.
She had significant discomfort with her day to day activities and still couldn’t load and unload her dishwasher without pain.
I will never forget the question she asked me during one of our visits.
“Why wasn’t this therapy available to me after surgery?”

No answer was good enough
It wasn’t the first time I had been asked that. In fact, I heard it so many times from my female patients who had been silently suffering with incontinence, pelvic pain, and bowel issues that I had mastered a scripted response by then.
It went something like this:
“Ah…yes. Well, we try to educate physicians on the benefits of referring to physical therapy early on to avoid complications…”
She interrupted me.
“You need to change this.”
I remember looking at her.
Like really looking at her.
And then looking away.
I didn’t immediately respond. To be honest, I don’t remember if I said anything at all that was worth a damn.

It was the first time, like real time, that someone held me personally accountable to end their suffering.
At least, that’s the way I took it.
My manager later on would tell me to not overthink it.
“You are doing the best you can. We all are. You are helping so many people….” and more of the same bullshit I can’t remember that healthcare providers tell themselves to justify the status quo of a broken system.
None of what she said to me wouldn’t make a difference.
In the end, I knew my patient was right.
It was my responsibility that the patients I treated were offered early access to rehabilitation after procedures performed on them like cesarean section and hysterectomy.
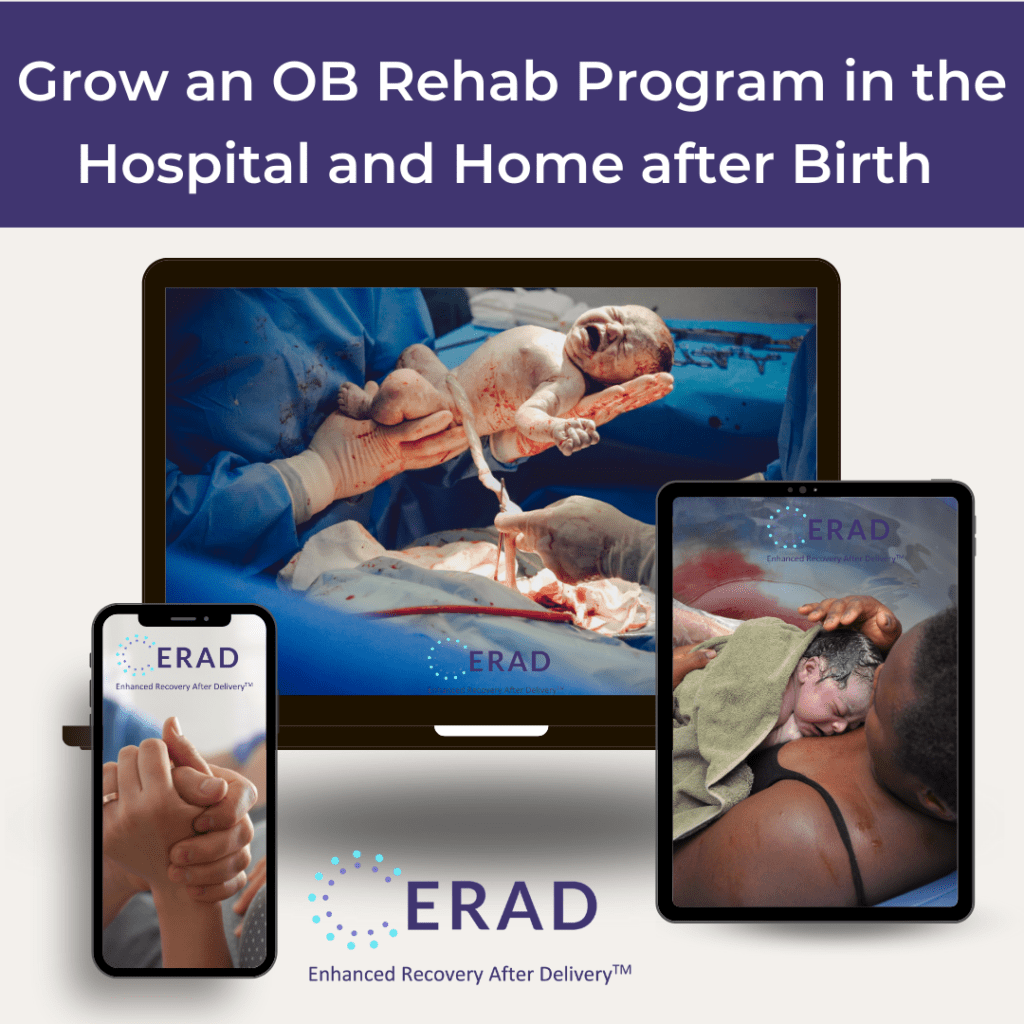
When I compared the length of recovery after female-specific surgeries like c-section and hysterectomy to the pelvic surgeries, general abdominal surgeries, and joint replacements that included men, women consistently had a longer recovery time than the patients who started therapy as early as the hospital stay.
In my own practice, I was treating men after pelvic surgery with rehab interventions that would improve their healing way earlier than I was offering these same treatments to women.
The most challenging endeavor I later encountered was changing the underlying culture that defined women’s function and recovery beyond my individual hospital system.
I started advocating for equitable access to rehabilitation after birth and surgery that directly impacted pelvic and women’s health.
The team I chose to work with helped individuals access hospital and home-based occupational and physical therapy after birth and pelvic surgery, which included marginalized groups such as Black women who had the highest rates of cesarean section and hysterectomy in the United States.
We took Action
In 2021, we started Enhanced Recovery After Delivery, a training pathway for healthcare providers to offer OT and PT in the hospital and home after birth.
In 2022, we started the Pelvic Health Network, an educational platform dedicated to making recovery options after birth, surgery, and for pelvic health conditions accessible to everyone.
In 2023, we launched the Women’s Health and Business Expo and started the Perinatal Health Specialist certification to retain a qualified workforce that would ensure equitable and early access to education and interventions to improve women’s health, function, and finances.
In 2024, we graduate our first cohort of Perinatal Health Specialists.
To be abundantly clear, standard pelvic health therapy is not unethical or demeaning to women.
However, the way I chose to practice in the past was.
Some of the most impactful individuals I have met on the planet are healthcare providers who treat pelvic floor dysfunction and women’s health conditions.
The takeaway message I want you to know was the way that I was preferentially treating men earlier than women was demeaning and unethical.
And I couldn’t live with that.
You Make This Possible
To the professionals who fight for the people you serve and prioritize what they want over protocols that are more harmful in the long run, I sincerely thank you.
For continued education on practices that prioritize individualized care rather than systematic protocols that never made sense in the first place, join us for one of the most impactful webinar the Pelvic Health Network will air to date.