
Breastfeeding strategies for birth professionals Q/A
Join our discussion with Dr. Ann Croghan about early intervention strategies that will help breastfeeding function and goals in the first 0 - 6 weeks of postpartum recovery. WATCH HERE
To view the replay of past events, use the calendar feature to go back to the date of the event.

Join our discussion with Dr. Ann Croghan about early intervention strategies that will help breastfeeding function and goals in the first 0 - 6 weeks of postpartum recovery. WATCH HERE
April 2, 2025 In hospitals across the country, rehab therapists routinely monitor vital signs with patients during the activity they are expected to perform at home. Dr. Jennifer Bonia, PT, DPT is an acute care therapist treating patients in the hospital after c-section who inspired this month's inaugural Women's Health Research Club on the use of the Adult Vital Sign Interpretation in Acute Care Guide to expand evidence-based rehab practice on the maternity unit. Join us HERE for a discussion on using this guide for immediate postpartum recovery care on Wednesday, April 2nd at 7:30 PM ET.

🏥 Postpartum pain has been closely linked with maternal mental health and studies have examined the impact of maternal pain on newborn bonding. 🩺 Dr. Addy Javes, PT, DPT shares her recent case report on the impact that physical therapy has in the hospital after birth on postpartum pain and function to improve maternal outcomes after cesarean section. 🗓️ Join us for an exclusive interview with her on why she wrote about this area of recovery care that’s rarely offered to new moms: Monday, May 12, 2025 at 8 PM ET. Watch the livestream HERE
As interest in maternal and pelvic health continues to rise in both acute care and home health settings, an increasing number of programs and businesses are introducing OT and PT services earlier than traditional standards of care. Join us for a dynamic roundtable discussion featuring occupational and physical therapy students, capstone advisors, and practicing clinicians. Together, they’ll explore how maternal and pelvic health are being redefined across hospital, home, and virtual care environments. REGISTER HERE
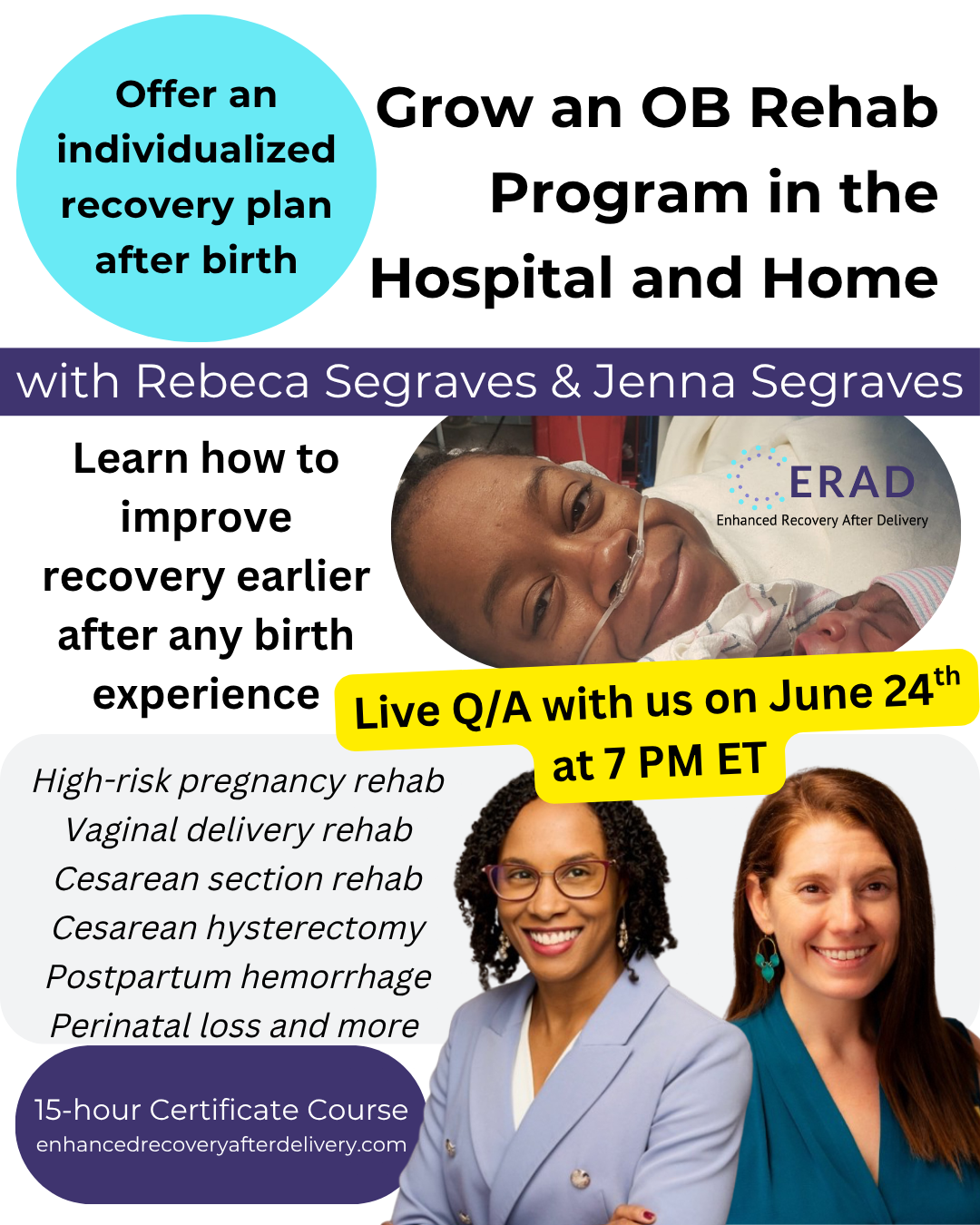
This special Q/A will be open to the public and to Pelvic Health Network members who have specific questions on starting a new service line, business, or hospital-based program that provides acute care, virtual, and home-health services during: pregnancy (including high-risk conditions) and within 0-6 days following any birth experience and pelvic surgery (e.g. hysterectomy, high-degree perineal tear, sterilization, hemorrhage management, and more). We will discuss the upcoming Enhanced Recovery After Delivery training that prepares licensed health providers and birth professionals to expedite maternal health support faster than the current standard of care. This training will be offered via livestream and in-person, providing breakfast, lunch, and a beautiful hike with iconic views of the Pikes Peak region. The training will be professionally recorded for future, self-paced participants while our livestream and in-person participants will master the hands-on techniques that can be started in the hospital and home. Every trainee will have access to a 1:1 meeting with an ERAD instructor that they can request within the 12 months from the start of their training: live or self-paced. This Q/A will answer your questions on whether or not you should continue observing perinatal health practice across all settings OR if you are ready to advance your career and join us at our beautiful headquarters in Colorado Springs on July 19-20, 2025. After this training, you can choose to pursue the Perinatal Health Specialist Certification that is 100% unique to this specialized area of practice. We can't wait to meet you, learn about your mission, and help you succeed! This Q/A will be recorded for members of Pelvic Health Network where memberships directly support program and professional development to advance early interventions in acute care, home health, virtual practice, and community-based support for maternal health, women's health, and pelvic health care. REGISTER HERE
Live Q/A for clinicians establishing rehab services as a standard of care during high-risk pregnancy and within the first 7 days postpartum to enhance recovery after any birth experience. Join us for a review of the Acute Care OB Rehab Manual with Spanish translation updates and resources for acute perinatal rehab program development + an introduction to the simple solution that's filling the gap between hospital and home: the Medbridge Birth Recovery Pathway. Coming September 2025. Register HERE
What is the difference between occupational therapy and physical therapy in maternal care? This is one of the most common questions we hear from providers, students, and hospital teams every year. The answer matters as maternal rehab becomes a greater priority in hospitals, clinics, telehealth, and home-based care. In this live panel discussion, experienced OTs and PTs will share how their roles overlap and where they are distinct in supporting recovery during pregnancy and after birth, including postpartum complications and Cesarean recovery. We will explore case examples from acute care, home health, and outpatient settings, and discuss how both professions can collaborate to improve function, safety, and quality of life for mothers. What you will learn: The scope of OT vs PT practice in maternal health Key similarities and differences in evaluation and treatment approaches How interprofessional collaboration improves recovery outcomes Real-world examples from hospital to home Bring your questions for a lively Q&A. Whether you are a provider, student, or administrator, this session will give you clarity on the unique and complementary roles of OT and PT in maternal care. REGISTER HERE
Some clinicians believe that any rehab setting outside of an outpatient women’s health clinic provides subpar care to mothers during pregnancy and after birth. But what happens when hospitalists, OB/GYNs, nurses, and other maternal health providers recognize the value of having a rehab professional on their care team during a high-risk pregnancy admission, or when a new mother is experiencing functional impairments before hospital discharge? What do you do when local providers want to start offering rehab services in the home within the first weeks of postpartum recovery, while mothers are still healing and bonding with their newborn? How do you respond when your hospital system wants to extend perinatal triage services through telehealth rehab to reduce postpartum readmissions and connect patients to earlier guidance on mobility and recovery? Would you say, “No. Refer your patients to me when they’re ready for outpatient women’s health rehab.” Of course not. In our monthly meeting, designed for Perinatal Health Specialist Certification members, we will answer live questions on how to build maternal rehab services across diverse settings to meet patients across the continuum of care and improve maternal health outcomes earlier than the current standard. Topics will include how to identify the right setting for the care a patient is seeking, strategies for building referral networks across disciplines, billing considerations, collaboration with other providers, and practical approaches to improving maternal function and recovery with earlier access to rehab. PHS-C Members: Bring your questions about clinical practice, program assignments, and connect certification objectives with real-life applications. REGISTER HERE
Diastasis Rectus Abdominis training is everywhere. Courses, books, and programs are being sold to both providers and the public. But if that information was enough, why are so many women still confused and stuck in slow recovery? In this episode I talk with Antony Lo, a physiotherapist from Australia who is known for challenging the way we think about abdominal muscle separation. He explains why memorizing anatomy, isolating muscles, changing breathing patterns, and prescribing low-level exercises may not be the best place to start. “By reframing what having DRA means, we have a chance of changing the experience for millions of women.” Antony teaches what that looks like in practice and why simple shifts in how we assess and guide movement can make a huge difference. If you think you already know everything about DRA, this conversation will push you to look again. And when his training is offered in your region, you will not want to miss it. Host, Rebeca Segraves, Pelvic Health Network WATCH HERE

💡 What if you could provide your patients with more options for recovery earlier than the standard of care? Across the country, patients recovering from cesarean delivery are sent home without early rehab or movement guidance. For some, even the surgery itself is painful: 11% to 14.6% experience pain during a C-section when anesthesia doesn't work effectively. Many more struggle with preventable pain, fatigue, and loss of function after birth. As surgery recovery professionals, we see how early rehab can change these outcomes. Yet, too often, clinicians are led to believe that "there isn't enough evidence" to support recovery care during the first six weeks after surgical birth. This webinar is an opportunity to change that. Join us to learn how to use evidence-informed tools and strategies that expand the movement choices patients have during pregnancy and early recovery so that every patient can participate in their healing and not just endure it. 📅 From Data to Delivery: Launching Your Virtual Rehab Practice Before and After Birth 🕖 Tuesday, November 4, 2025 at 7 PM ET 🎁 Bonus for Attendees: All registrants will receive an evidence-informed movement guide that includes sample birth preparation and early recovery movements with explanations of their purpose and benefits. The guide helps clinicians expand patient options for movement, autonomy, and participation in recovery. 🩺Purpose with impact: Thirty percent of proceeds will fund research on early rehabilitation after surgical births, including perineal repairs and cesarean deliveries. Research on early rehab after birth will help every clinician who has been told there isn't enough evidence to start sooner. If you're ready to lead the change in how early recovery care after birth begins, join the movement. REGISTER HERE
How can rehabilitation professionals enhance postpartum recovery during the first six weeks after birth across hospitals, home, virtual, and clinic settings? Enhanced Recovery After Delivery® (ERAD®) is an evidence-informed pathway focused on improving recovery during the earliest and most vulnerable phase after childbirth. This monthly information session is designed for occupational and physical therapists and healthcare leaders who want to strengthen postpartum recovery within hospitals and extend care beyond discharge into home-based, virtual, and outpatient settings. In this session, we will discuss: Why the first six weeks postpartum are critical for function, safety, and long-term outcomes How inpatient rehabilitation is being integrated into maternity care and positioned as the starting point for recovery How hospitals and clinics are building continuity with home-based, virtual, and outpatient postpartum rehab services What early recovery looks like after different birth experiences, including cesarean birth, postpartum hemorrhage, perineal trauma, high-risk pregnancy admissions, and perinatal loss How rehabilitation professionals are advancing their role from direct care to program development and system-level impact This session will also introduce the ERAD® training and leadership pathways available to clinicians and hospitals interested in developing or expanding early postpartum rehabilitation services. REGISTER HERE